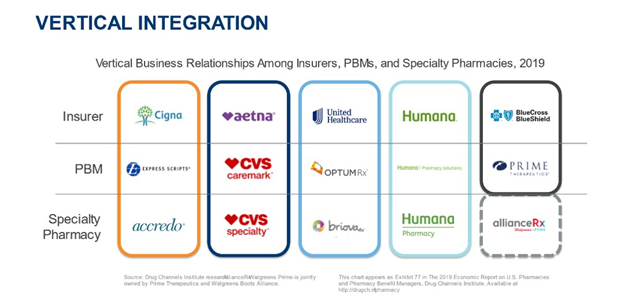
Vertical relationships between the nation’s largest payors, pharmacy benefit managers (PBMs), and specialty pharmacies create barriers for hospitals and health systems to access the payor landscape. Some, but not all payors have expanded their vertical integration to include retail pharmacy, infusion, nursing, durable medical equipment, and more.
Vertical integration has resulted in the largest payors pushing business to themselves and restricting access to those outside the payor silo. Within the current landscape, how do hospital/health system pharmacies gain access to payor networks, especially when it comes to specialty pharmacy?
Strategies to Gain Access to Payor Networks
Opportunities exist to access networks with payors that are not yet fully vertically integrated. Let’s look at some key strategy points when approaching these payors.
- Identify payor plans that have similarly aligned incentives as the hospital/health system.
- Identify leverage points such as location that can be used to negotiate with payors. A rural hospital may be the only facility in a geographical region, making it an attractive connection for payors.
- Identify what makes the hospital/health system unique and desirable to the payor. What can the hospital/health system provide the payor that it cannot get on its own, such as outcomes and data? Is the facility an accountable care organization (ACO)? If so, communicate that the facility needs to be in the payor network to manage risk and drive positive patient outcomes.
Benefits of Having a Partner to Access Payor Networks
Medical and pharmacy benefits have been in separate buckets for years, creating a communications barrier that can be challenging to overcome. Consequently, most hospitals/health systems have very good medical relationships but often are not as experienced in pharmacy contracting.
A partner with expertise in payor access can leverage medical relationships within the payor PBM to navigate and achieve payor access. Once established, that partner can coach the hospital/health system pharmacy in the process going forward.
The right partner can also help overcome barriers to entry in setting up specialty pharmacy by:
- Facilitating dual accreditation, which is necessary for gaining payor network access for specialty drugs
- Guiding the facility through setting up a specialty pharmacy separate from the in-house retail pharmacy
Selecting the right partner can cut the time to gaining payor access for specialty drugs by 50% once dual accreditation is established.
Case Studies
Let’s take a look at some case studies that illustrate how partnering with SPARx resulted in achieving payor access.
A multi-site system in the Midwest
The payor informed the hospital that they would not be able to administer infusions in the hospital due to a site of care issue resulting in loss of the infusion business. However, the payor would allow the facility to administer infusions at the hospital if the hospital established a specialty pharmacy. By working with SPARx to build a specialty pharmacy in-house, the hospital was able to retain the infusion business and establish a specialty network.
Two health systems with existing in-house specialty pharmacies
Both facilities, one on the East coast and one on the West coast, had operated specialty pharmacies for a number of years, but the business had stagnated due to lack of payor access.
- Hospital 1 is located in an “any willing provider state” but still had challenges getting into networks. SPARx helped the facility leverage the right contacts to gain network access.
- Hospital 2 is located in a “non-willing provider state” and needed help identifying their leverage points, establishing full service, and more. By partnering with SPARx, this facility also gained payor access and grew its specialty pharmacy business.
